The Credo Health report brings together survey findings from 500+ physicians and care team members, insights from a 150+ clinician point-of-care beta, and real-world pilot evidence on what drives action in clinical workflows, especially in Medicare populations where care is distributed across more settings, more clinicians, and more transitions.
DENVER, Feb. 5, 2026 /PRNewswire-PRWeb/ -- Credo Health today released a new report, "Closing the Data to Action Gap in Value Based Care (VBC)," detailing how gaps in access to patient health records cost the U.S. healthcare system ~$8B annually, and the impact AI can have in closing that gap.
The report brings together survey findings from 500+ physicians and care team members, insights from a 150+ clinician point-of-care beta, and real-world pilot evidence on what drives action in clinical workflows, especially in Medicare populations where care is distributed across more settings, more clinicians, and more transitions.
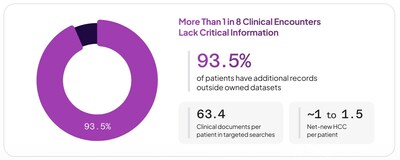
Credo's analysis estimates missing medical records drive an estimated ~$8B per year in operational waste from lost specialist capacity and primary-care disruption; ~20,000 deaths and ~1.5M delayed or missed diagnoses associated with incomplete clinical context; and ~$1,100 per Medicare patient per year in missed risk-based revenue opportunity tied to RAF and documentation gaps.
"Our mission at Credo Health is to help doctors perfectly diagnose and treat every patient," said Carm Huntress, CEO of Credo Health. "We saw VBC performance improve when clinicians had decision-ready context at the point of care. In our beta, physicians used an AI copilot to review more complete clinical histories, with clinically supported care opportunities (suspected HCC conditions for Medicare risk adjustment) surfaced by Credo's AI agents for medical record acquisition and analysis. That made it far easier to review information, extract insights, and take action."
Deep dive: Why VBC struggles at the point of care
Despite major investments in interoperability, the multi-sourced analysis in the report finds that record completeness and usability remain inconsistent in day-to-day workflows, forcing clinicians to hunt across notes, PDFs, labs, consult letters, and external packets to test hypotheses and make decisions. This "last mile" problem is especially acute in Medicare populations with multiple chronic conditions.
"Physicians have always used data to form and test hypotheses. They ask layered questions and hunt for evidence to validate or challenge an assumption," said Avishaan Singh Sethi, CTO of Credo Health. "In theory, more data and more technology should make that easier, but - increasingly - the opposite has been true. With critical, unstructured records scattered across systems, clinicians often feel less confident they're seeing the full picture. In our pilot, closing the data-to-action gap required pairing physicians with AI engineers so the AI could be trained to assemble and structure data, generate clinically relevant insights, and answer the detailed, layered questions physicians need to ask to feel confident in taking action."
Pilot evidence: completeness + evidence-backed insights drive clinician action
In a pilot with a large value-based primary care organization (a ~500-patient cohort reviewed by two different solution providers), Credo's physician-trained suspecting model produced 2.1× more clinically accepted net-new HCC suspects: physicians accepted 425 net-new suspects from Credo (77%) compared with 200 net-new suspects from the competing solution (66%). The difference was Credo's ability to surface source-verifiable clinical opportunities that were easier for physicians to review and trust at the point of care.
"AI models get significantly more effective when we're able to train them in the way physicians reason through a patient record," said Joshua Solot, MD, Consulting Physician, at Credo Health. "When the AI can show its work, trust and usability at the point of care increase and translate into meaningful clinical actions that can ultimately save lives."
The impact: better data only matters if it earns trust and reduces work
The report underscores a parallel reality: clinicians are already operating at capacity. Reviewing and synthesizing incomplete patient histories competes with heavy EHR workloads and contributes to burnout. As a result, the bar for AI in VBC is not accuracy alone, but whether it reduces burden and helps clinicians make decisions more easily, in the moment that care is delivered.
What the report outlines
- Gaps and challenges in digital chart acquisition to assemble longitudinal records across sources, not just a single feed
- How clinically trained AI extracts decision-relevant insights with source-cited evidence clinicians can verify
- The impact of artifact-ready outputs clinicians can copy into documentation, prior authorization support, and risk and quality workflows
- Timelines and trend views that surface what changed, what is unstable, and what is missing
Availability
The report, "Closing the Data to Action Gap in Value Based Care," is available now at: Closing the Data to Action Gap
Key findings
- VBC execution breaks when clinicians can't get decision-ready context fast enough to act at the point of care.
- Record fragmentation and workflow constraints mean interoperability alone doesn't guarantee completeness.
- Pilot results show evidence-backed, source-cited insights can increase clinician adoption and acceptance at the point of care.
- AI must be designed to reduce burden: fast, source-verifiable, clinically relevant, and immediately usable.
Media Contact
Nate Purpura, Credo Health Solutions, Inc., 1 8052153336, [email protected], CredoHealth.com
SOURCE Credo Health Solutions, Inc.



Share this article